Establishing Relationships with Patients' Families
Building relationships with patients' families is an essential aspect of nursing practice that goes beyond medical care but is equally important. It is an integral part of the job, balancing empathy and professionalism daily. In the North, additional challenges complicate this delicate balance: language barriers, the influence of the community, and differing values. Here are some tips to establish trust with families to ensure the well-being of your patients.
Open-mindedness and Patience in Engaging with Patients' Families
Patients in these communities often practice traditional medicine and use natural remedies. Traditional medicine and natural remedies may be more accessible and affordable than biomedical care, especially in remote areas. Patients might also have greater trust in traditional practitioners, who are often community members sharing similar cultural values and beliefs. Traditional medicine often considers health more holistically than biomedical care, accounting for physical, mental, spiritual, and social well-being. It is important to be receptive and understanding, and not to dismiss these practices. Sometimes, you may need to reconcile modern and traditional medicine, so it’s important to be open-minded. By actively listening to the family's concerns, ensure they know you understand and consider their legitimate worries. This helps build mutual trust. By adopting a culturally sensitive and patient-centered approach, you can establish a strong, trusting relationship with patients from diverse communities, offering them quality care and improving their overall well-being.
Language Barriers
Communication, empathy, respect, and adaptation are fundamental elements in establishing a solid trust relationship with patients, leading to better understanding, shared decision-making, and improved health outcomes.
While many Indigenous people speak English, not all do. They also rely heavily on non-verbal communication in addition to English. Paying attention to their facial expressions and confirming your understanding is crucial. For example, a frown from an Inuit person signifies "no," while a raised eyebrow simply means "yes."
Jessica, a nurse at Premier Soin Nordik, shares her experience: “Besides the medical staff, the people working at the clinic (janitors, secretaries, archivists, etc.) are community members and speak both English and the Indigenous language. If there is a patient who only speaks their Indigenous language, we work with an available staff member. Personally, I have never encountered someone who doesn’t understand English at all. Children must be accompanied until age 14, and elderly patients are often accompanied by a family member.” Although patients are usually accompanied by an English-speaking relative, this complicates patient assessments. Effective understanding and communication become difficult, especially when giving information, instructions, or education.
Being open and sensitive to cultural differences and trying to adapt is crucial for building a trust relationship with patients, such as by learning a few words in their language. Here you can find resources for learning Indigenous languages.
Intergenerational Relationships Matter
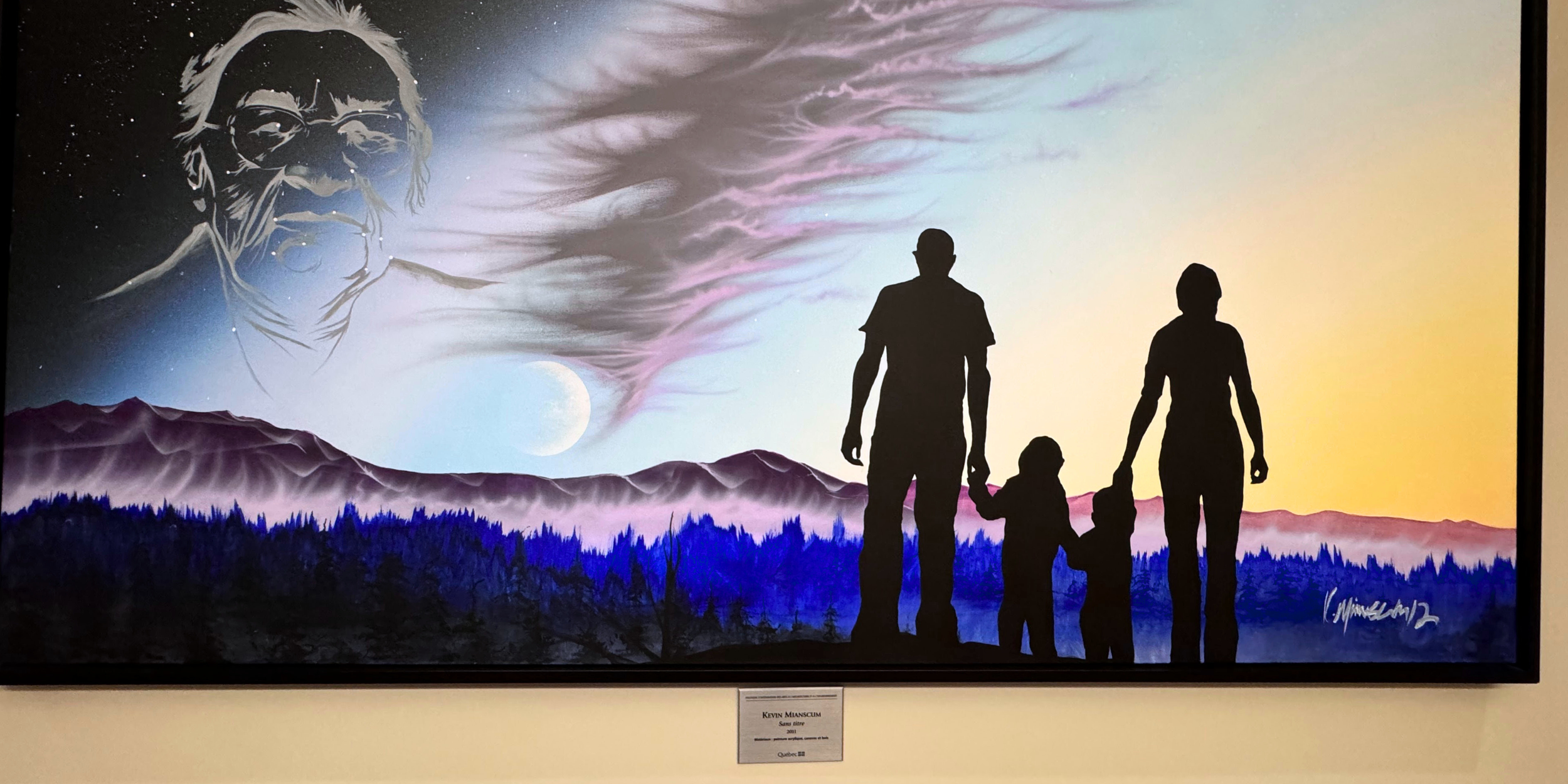
Indigenous peoples, being community-oriented societies with hierarchical structures and defined roles, place great importance on community in family interactions. For example, the elder’s opinion often holds significant weight in some communities. Young people frequently consult their grandparents for important decisions, including health matters, where traditional medicine is often favored. Recognizing this dynamic and valuing intergenerational relationships in exchanges with patients’ families is crucial.
In this context, establishing trust with patients' families becomes even more important. For example, patients are often accompanied during consultations, and in emergencies, multiple family members may be present to support the patient. Adapting to these situations, even in confined spaces, and delicately finding compromises is essential to preserve trust. This involvement of patients' families in care also provides valuable insights into family dynamics, enhancing the quality of care provided.
Involving Patients' Families in Care
One of the most important rules in the nursing code of ethics is respecting the confidentiality of medical data. You must reassure families while upholding this duty. To build this trust, try involving family members when possible.
Jessica, a nurse in the Far North, shares an experience: In Indigenous culture, time spent in nature, like hunting periods, is very important. If a patient needs to return to the clinic daily for wound dressing changes, they might skip weekends to spend time in the woods outside the village. In such cases, we can adapt to ensure the patient receives the best care under the circumstances. For example, we might reassess the need for dressing changes on weekends or provide the patient or a family member with the necessary supplies and teach them how to do the dressing themselves. This approach optimizes wound care by actively involving the patient or their family in the care process. It not only improves treatment effectiveness but also builds trust with the patient and their family, facilitating communication and collaboration in future care stages.
Adapting Communication
When communicating with patients or their families, avoid complex medical jargon to ensure they fully understand crucial health information. Use clear and simple terms to better involve relatives, allowing for better collaboration and informed decision-making—essential values for the nursing profession.
Providing clear and comprehensive written documents summarizing the care plan, medications, and other relevant information allows the family to easily refer to them at any time. This promotes better understanding and encourages active involvement in the patient's care. This open and transparent approach helps build trust and collaboration with the family.
Cultivating Open-mindedness
Prioritize open and transparent communication with the patient's family, remaining available to answer their questions with empathy and expertise. Ensure regular and personalized follow-up with the family, taking the time to address their concerns and adjust the care plan based on the patient's evolving needs. This holistic and patient-centered approach fosters optimal care and better family involvement. By contributing to creating an environment conducive to quality care, you will offer a positive experience to both the family and the patient. Are you ready to join the adventure? Want to join the adventure?